trauma and the brain pdf
The Impact of Trauma on the Brain
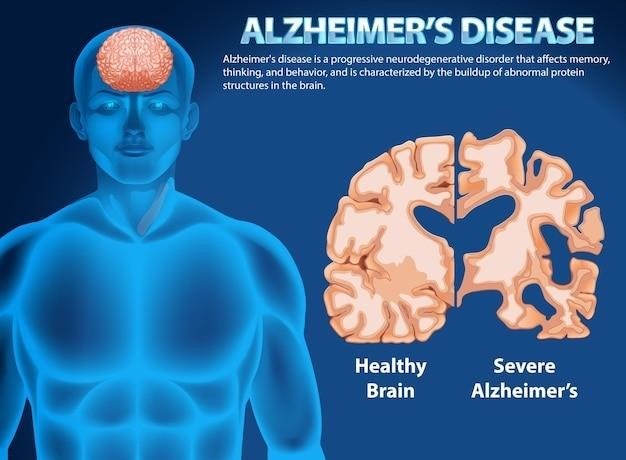
Trauma can have a profound impact on the brain‚ leading to lasting changes in structure and function․ These changes can affect a person’s emotional regulation‚ cognitive abilities‚ and overall well-being․ The brain’s remarkable plasticity allows it to adapt to various experiences‚ including trauma‚ but these adaptations can sometimes be maladaptive and contribute to long-term difficulties․
Brain Regions Affected by Trauma
Trauma can significantly impact various regions of the brain‚ leading to alterations in their structure and function․ The hippocampus‚ responsible for memory formation and retrieval‚ may be affected‚ leading to difficulties recalling traumatic events or forming new memories․ The amygdala‚ the brain’s fear center‚ can become hyperactive‚ leading to heightened anxiety and fear responses․ The prefrontal cortex‚ responsible for executive functions like decision-making and emotional regulation‚ may also be affected‚ contributing to difficulties with impulse control‚ planning‚ and problem-solving․
The Hippocampus
The hippocampus plays a crucial role in memory formation and retrieval‚ particularly for explicit memories‚ which are conscious recollections of events and facts․ Trauma can disrupt hippocampal function‚ leading to difficulties recalling traumatic experiences or forming new memories․ This disruption can be due to the release of stress hormones like cortisol‚ which can damage hippocampal cells․ Research suggests that the hippocampus may also be involved in the development of post-traumatic stress disorder (PTSD)‚ as it plays a role in emotional processing and regulation․
The Amygdala
The amygdala is a brain region crucial for processing emotions‚ particularly fear and anxiety․ It plays a key role in the “fight-or-flight” response‚ triggering physiological changes in response to perceived threats․ Trauma can lead to hyperactivation of the amygdala‚ making individuals more sensitive to perceived threats and prone to experiencing anxiety and fear․ This hyperactivation can also contribute to the development of PTSD‚ as the amygdala becomes overly sensitive to cues associated with the traumatic event‚ triggering fear and anxiety responses even in the absence of actual danger․
The Prefrontal Cortex
The prefrontal cortex‚ located at the front of the brain‚ is responsible for higher-level cognitive functions such as planning‚ decision-making‚ impulse control‚ and emotional regulation․ Trauma can disrupt the prefrontal cortex’s ability to effectively regulate emotions‚ leading to difficulties with controlling impulses‚ managing stress‚ and making rational decisions․ This can manifest as impulsive behaviors‚ difficulty concentrating‚ and challenges with emotional regulation‚ contributing to various mental health challenges‚ including anxiety‚ depression‚ and PTSD․
Trauma and Brain Development
Traumatic experiences during childhood can have a profound impact on brain development‚ shaping how a child’s brain processes emotions‚ regulates stress‚ and interacts with the world․
The Stress Acceleration Model
The stress acceleration model suggests that exposure to chronic stress‚ particularly during childhood‚ can accelerate the maturation of the brain’s threat system․ This system‚ responsible for detecting and responding to danger‚ becomes hyper-vigilant in response to trauma‚ leading to heightened anxiety‚ fear‚ and reactivity․ While this may have been adaptive in a threatening environment‚ it can become maladaptive in a safe environment‚ leading to difficulties in daily life and increased vulnerability to mental health challenges․
The Impact of Abuse vs․ Neglect
While both abuse and neglect can have significant impacts on brain development‚ research suggests that abuse may have a greater impact on the brain’s threat system․ Abuse‚ which involves direct harm or threat‚ triggers stronger stress responses and can lead to more pronounced changes in brain regions involved in fear processing‚ emotional regulation‚ and social cognition․ Neglect‚ while also detrimental‚ may have a more subtle impact on brain development‚ often affecting areas related to attachment‚ self-regulation‚ and cognitive development․
Brain Plasticity and Recovery
The brain’s remarkable plasticity allows it to adapt to various experiences‚ including trauma․ This means that even after trauma‚ the brain can change and reorganize itself‚ potentially leading to recovery․ However‚ the extent of recovery depends on various factors‚ including the severity of the trauma‚ the individual’s resilience‚ and the support they receive․ While some changes may be permanent‚ research suggests that interventions like therapy‚ support groups‚ and other forms of treatment can help facilitate brain healing and improve long-term outcomes․
Trauma-Informed Care
Trauma-informed care (TIC) is a framework that recognizes the widespread impact of trauma and incorporates knowledge about its effects into policies‚ procedures‚ and practices․
Understanding Trauma Responses
Trauma responses are highly individualized and can manifest in various ways․ Some individuals may experience hyperarousal‚ characterized by increased vigilance‚ anxiety‚ and difficulty relaxing․ Others may exhibit avoidance behaviors‚ withdrawing from social situations or activities that trigger memories of the trauma․ Some people may experience dissociation‚ feeling detached from their surroundings or their own body․ It’s crucial to understand that these responses are not signs of weakness but rather adaptive mechanisms developed to cope with overwhelming experiences․
The Role of Trauma in Treatment
Trauma plays a significant role in treatment‚ impacting both the therapeutic process and the patient’s response to interventions․ Understanding the impact of trauma on a patient’s life‚ including their experiences‚ symptoms‚ and coping mechanisms‚ is essential for effective treatment․ Trauma-informed care involves recognizing the potential presence of trauma‚ understanding its effects‚ and integrating this knowledge into all aspects of treatment․ By adopting a trauma-informed approach‚ providers can create a safe and supportive environment that fosters trust and facilitates healing․
Best Practices for Trauma Patients
Best practices for trauma patients emphasize a holistic approach that addresses the multifaceted needs of individuals who have experienced trauma․ This includes creating a safe and supportive environment that minimizes retraumatization‚ building trust and rapport with the patient‚ and providing tailored interventions that address their specific needs․ These interventions may include individual or group therapy‚ medication management‚ and skills training to manage symptoms such as anxiety‚ depression‚ and post-traumatic stress disorder․ It is crucial to recognize that healing from trauma is a journey‚ and patience‚ compassion‚ and a collaborative approach are essential for successful outcomes․
Traumatic Brain Injury (TBI)
Traumatic brain injury (TBI) is a serious condition that can occur when the brain is injured due to an external force․ This injury can range from mild to severe‚ and the effects can be long-lasting․
Types of TBI
Traumatic brain injuries (TBIs) are categorized based on the severity of the injury and the mechanism of impact․ A mild traumatic brain injury (mTBI)‚ also known as a concussion‚ is the most common type of TBI․ It is characterized by a temporary loss of consciousness‚ confusion‚ or disorientation․ Moderate TBI involves a longer period of unconsciousness‚ confusion‚ or memory loss․ Severe TBI is the most serious type and involves prolonged unconsciousness‚ coma‚ and significant neurological damage․ TBIs can also be classified as closed or penetrating․ Closed head injuries occur when the skull remains intact‚ while penetrating injuries involve an object piercing the skull and entering the brain tissue․
Symptoms of TBI
The symptoms of a TBI can vary widely depending on the severity and location of the injury․ Common symptoms include headaches‚ dizziness‚ nausea‚ vomiting‚ confusion‚ memory problems‚ difficulty concentrating‚ fatigue‚ sleep disturbances‚ irritability‚ and mood swings․ Some individuals may experience more severe symptoms such as seizures‚ loss of consciousness‚ paralysis‚ or coma․ The symptoms of a TBI can appear immediately after the injury or develop gradually over time․ It is important to seek medical attention if you suspect you or someone you know has sustained a TBI․
Treatment for TBI
Treatment for TBI depends on the severity of the injury and the individual’s specific needs․ Initial treatment often involves stabilizing the patient‚ managing any immediate medical complications‚ and preventing further brain injury․ Rehabilitation plays a crucial role in recovery and may include physical therapy‚ occupational therapy‚ speech therapy‚ and cognitive therapy․ Medications may be used to manage symptoms such as headaches‚ seizures‚ and anxiety․ The goal of treatment is to help individuals regain as much function as possible and live fulfilling lives despite their injuries․
Research on Trauma and the Brain
Research on trauma and the brain is rapidly expanding‚ seeking to understand the complex interplay between traumatic experiences and brain function․
Neurobiological Markers
Researchers are actively investigating neurobiological markers of trauma‚ aiming to identify specific changes in the brain that can help diagnose and understand the impact of trauma․ These markers may include alterations in brain structure‚ function‚ or neurochemical activity․ For example‚ studies have shown that individuals with a history of trauma may exhibit smaller hippocampal volumes‚ which is associated with memory and emotional regulation․ Additionally‚ changes in the levels of stress hormones like cortisol and norepinephrine have been observed in individuals who have experienced trauma․
Evidence-Based Therapies
The field of trauma treatment has made significant strides in developing evidence-based therapies that address the neurobiological and psychological impacts of trauma․ These therapies are supported by research and have demonstrated effectiveness in improving symptoms and promoting healing․ Cognitive-behavioral therapy (CBT) is a widely used approach that helps individuals identify and modify negative thought patterns and behaviors that contribute to distress․ Other evidence-based therapies include Eye Movement Desensitization and Reprocessing (EMDR)‚ which utilizes eye movements to process traumatic memories‚ and Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)‚ which combines CBT with elements of attachment-based therapy․
Future Directions for Research
The field of trauma and the brain is constantly evolving‚ with ongoing research exploring new avenues for understanding and treating the effects of trauma․ Future research directions include investigating the role of epigenetics in trauma-related brain changes‚ exploring the potential of personalized interventions based on individual brain responses‚ and developing novel biomarkers to identify individuals at risk for developing trauma-related mental health conditions․ Further research is also needed to understand the long-term effects of trauma on brain development‚ particularly in children and adolescents‚ and to develop effective interventions for preventing and treating trauma-related disorders․
